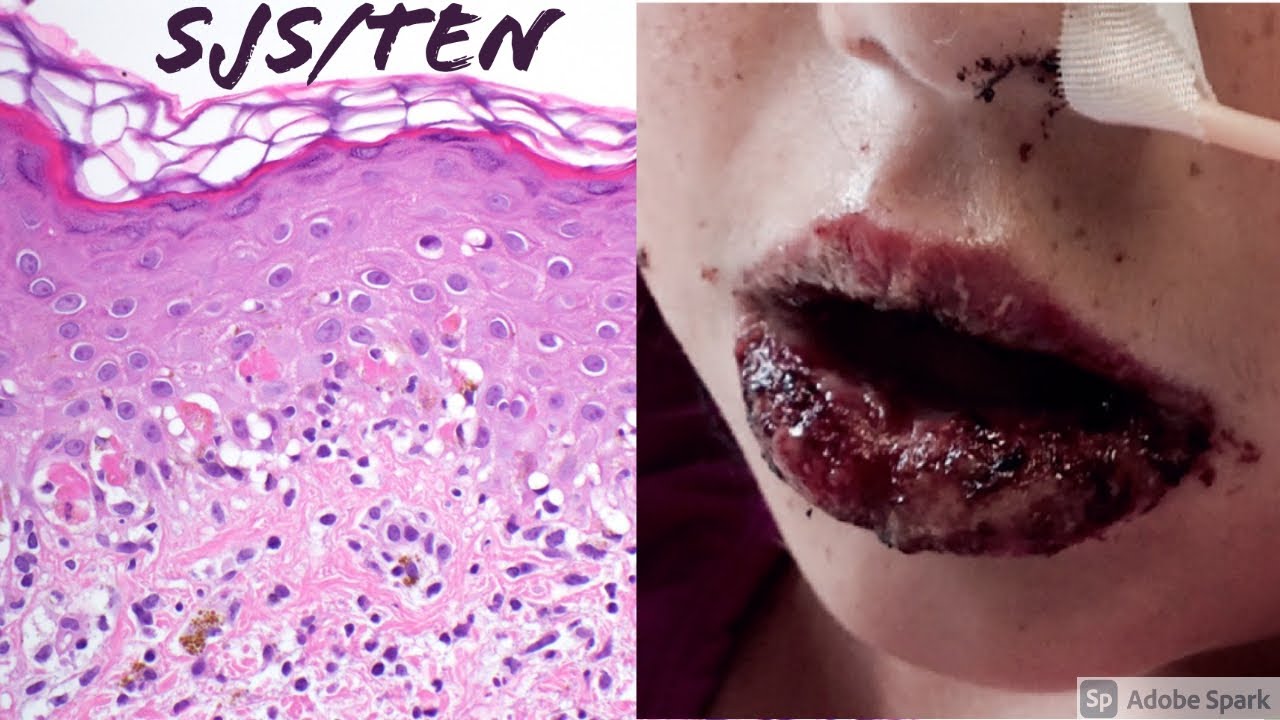
Understanding Toxic Epidermal Necrolysis: Causes and Consequences
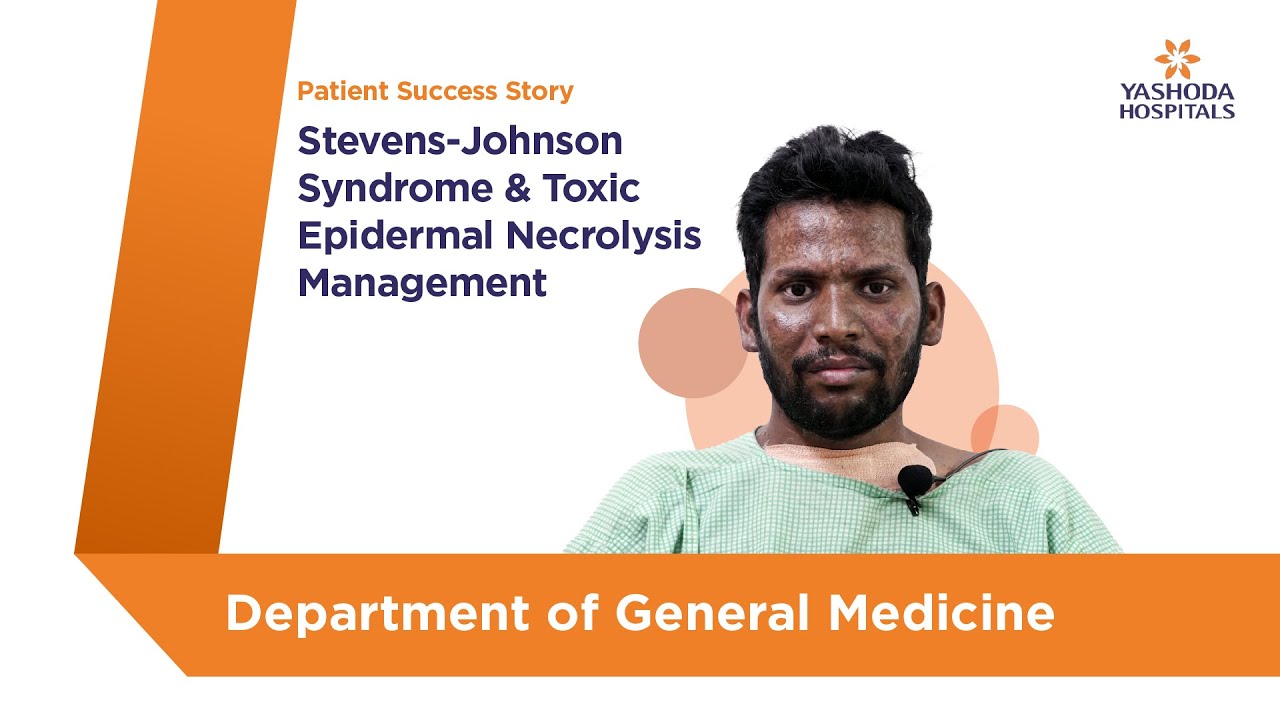
Toxic epidermal necrolysis (TEN) is a rare skin condition that can hit you hard, leading to severe damage to your skin and mucous membranes. It’s no joke—this condition often comes out of nowhere, frequently triggered by medications or infections. With TEN, your skin can detach itself in large areas, and that’s just the beginning of the complications that follow. We’re diving deep into the nitty-gritty of toxic epidermal necrolysis, so you know what you’re up against—what causes it, the consequences of living with it, and how to manage it.
When this condition strikes, the physical toll can be devastating. Imagine your skin peeling apart like sunburn, leading to extensive sores and widespread pain. But don’t get it twisted—the damage doesn’t stop with the skin. The psychological burden can be immense. People suffering from TEN often have to navigate emotional hurdles as serious as the physical ones. Understanding the full scope of toxic epidermal necrolysis means recognizing its profound impact on both body and mind.
But don’t worry, folks! Just like hitting the gym and smashing your fitness goals, there are ways to get through this. It’s important to know about TEN so you can avoid it if you can, catch it early if you can’t, and tackle it like a champ. You’ve already put in the hard work to build your muscles; now it’s time to build your knowledge.
Top 7 Causes of Toxic Epidermal Necrolysis: What You Need to Know
1. Medications
Not all medications are friendly; some can unleash toxic epidermal necrolysis. Sulfonamides like Bactrim, allopurinol for gout, and even oxycodone are familiar offenders. The big takeaway? Stay on guard when starting a new medication, and communicate with your healthcare provider about any prior drug reactions.
2. Infections
Believe it or not, infections can kickstart TEN. Viral infections such as the herpes simplex virus or mycoplasma pneumonia are common culprits. When you’re already dealing with health issues, you definitely don’t want an infection to complicate things and possibly lead to conditions like pyelonephritis.
3. Erythromycin Use
Erythromycin is usually a go-to antibiotic, but it’s got a dark side. Rarely, it can lead to toxic epidermal necrolysis, especially when used topically like in erythromycin ophthalmic ointment. If you have drug sensitivities, keep an eagle eye on any changes to your skin.
4. Autoimmune Disorders
Individuals with autoimmune conditions, such as lupus erythematosus, may find themselves at higher risk for TEN. That means if you’re dealing with these kinds of health issues, you need to be extra cautious about treatments and potential flare-ups.
5. Leukocytosis
A high white blood cell count, or leukocytosis, often signals an underlying issue—like medication reactions or infections. Monitoring blood parameters can’t be overstated if you’re looking to avoid conditions like TEN. It’s crucial for anyone who has a history of these ailments.
6. Previous History of TEN
Got hit with toxic epidermal necrolysis once? You’re in the danger zone for future episodes. Remember, once is often too many, so meticulous reviews of your drug history are vital. Avoid those offenders at all costs.
7. Sensitization to Environmental Factors
While not as common, environmental triggers can also spark TEN—think chemicals in the workplace. If your job puts you in contact with harsh substances, awareness is your best ally.
The Psychological Impact: Catastrophizing and Its Effects
The price of toxic epidermal necrolysis isn’t merely physical. As if going through the skin detachment wasn’t enough, the psychological toll can be just as hard-hitting. Many patients fall into the trap of catastrophizing, imagining the worst possible outcomes. This mindset can create a barrier to seeking help and adhering to treatment.
Imagine walking into the gym, but every time you see a weight, you think about the potential for injury instead of taking that challenge head-on. The same goes for those dealing with TEN. This kind of negative thinking can prolong suffering and delay recovery. That’s why tackling mental health is crucial.
Employing therapies like cognitive behavioral therapy (CBT) can help turn that negative mindset around. Getting mentally fit is just as important as training your body. Drawing strength from both the mental and physical sides will put you on the fast track to recovery.

Treatment Approaches and Management Strategies
Dealing with toxic epidermal necrolysis requires a solid game plan. You can’t just wish it away. Here’s how to tackle it head-on:
1. Immediate Intervention
Catching TEN early is the name of the game. Once diagnosed, the first step is to stop using the offending agent! Often, patients need to be admitted to specialized burn units for constant observation.
2. Supportive Care
You’ll want to focus on fluid resuscitation, pain management, and avoiding infections while dealing with TEN. Antibiotics might come into play to prevent complications like leukocytosis or pyelonephritis.
3. Immune Modulation
If the situation is severe, treatments may involve corticosteroids or immunoglobulin therapy. This helps dial back your immune system’s overreaction, aiming to curb skin necrosis.
4. Long-Term Follow-up
Once you beat TEN, the journey isn’t quite over. Continuous follow-ups are essential for managing scarring and preventing future complications. Your skin will need attention to stay healthy.
5. Patient Education
Knowledge is power! Teaching patients and their families about early signs of TEN is vital. Open conversations with healthcare providers about past drug reactions can help avoid reliving this nightmare.

Final Thoughts: Embracing a Holistic Approach
Toxic epidermal necrolysis is more than skin deep. To effectively manage it, you need a holistic approach that looks at both the physical and emotional dimensions. Knowing the causes and impacts of TEN helps healthcare professionals set you up for a better recovery.
Just like training for your best body, recovery requires a full commitment. A strong support system, education, and a positive mindset can make all the difference in dealing with this intense condition. It may feel like an uphill battle, but with awareness and determination, you can rise above toxic epidermal necrolysis and reclaim your life. So stay informed, stay strong, and always be your best advocate. You’ve got this!
Toxic Epidermal Necrolysis: Fun Trivia and Interesting Facts
Understanding the Basics
Toxic epidermal necrolysis (TEN) is a rare but serious condition that causes the skin to blister and peel off, resembling the aftermath of a severe burn. This condition can be triggered by medications, infections, or even the body’s immune response. Speaking of skin conditions, did you know that the term skunk hair refers to a peculiar look that some people achieve by dyeing their hair in bold, contrasting colors? Just like how one stands out with a striking hairstyle, those with toxic epidermal necrolysis find themselves in a very challenging and visible situation.
Causes and Symptoms
Interestingly, medications like non-steroidal anti-inflammatory drugs (NSAIDs) and certain antibiotics are common culprits behind toxic epidermal necrolysis. Much like the relationship between chronic diarrhea and dehydration, neglecting to address symptoms can lead to further complications. In fact, some patients might experience symptoms that escalate rapidly, such as flu-like signs followed by painful blisters. You’ve got to stay alert! It’s crucial to navigate these symptoms early because, without prompt treatment, the condition can worsen dramatically—almost akin to a horror film where a character’s plight intensifies every minute.
Awareness and Research
As the awareness surrounding toxic epidermal necrolysis grows, researchers are consistently conducting studies to get a better handle on this painful condition. Did you know that filmmaker George bianchini is an advocate for raising awareness about various medical conditions through creative storytelling? This direct connection emphasizes how storytelling can play a pivotal role in elucidating complex topics like health issues. Similarly, venues like the Kohl Center serve as platforms for community discussions and events that can spotlight lesser-known conditions, helping to educate the public on matters that affect individuals profoundly.
In summary, grappling with toxic epidermal necrolysis is no small feat. It’s essential to highlight such conditions, not just from a medical standpoint but also to appreciate the broader implications they have on daily life. So the next time you hear someone talk about flaky skin or debilitating symptoms resembling those of a movie disaster, remember that behind every ailment like toxic epidermal necrolysis lies a story worth telling.