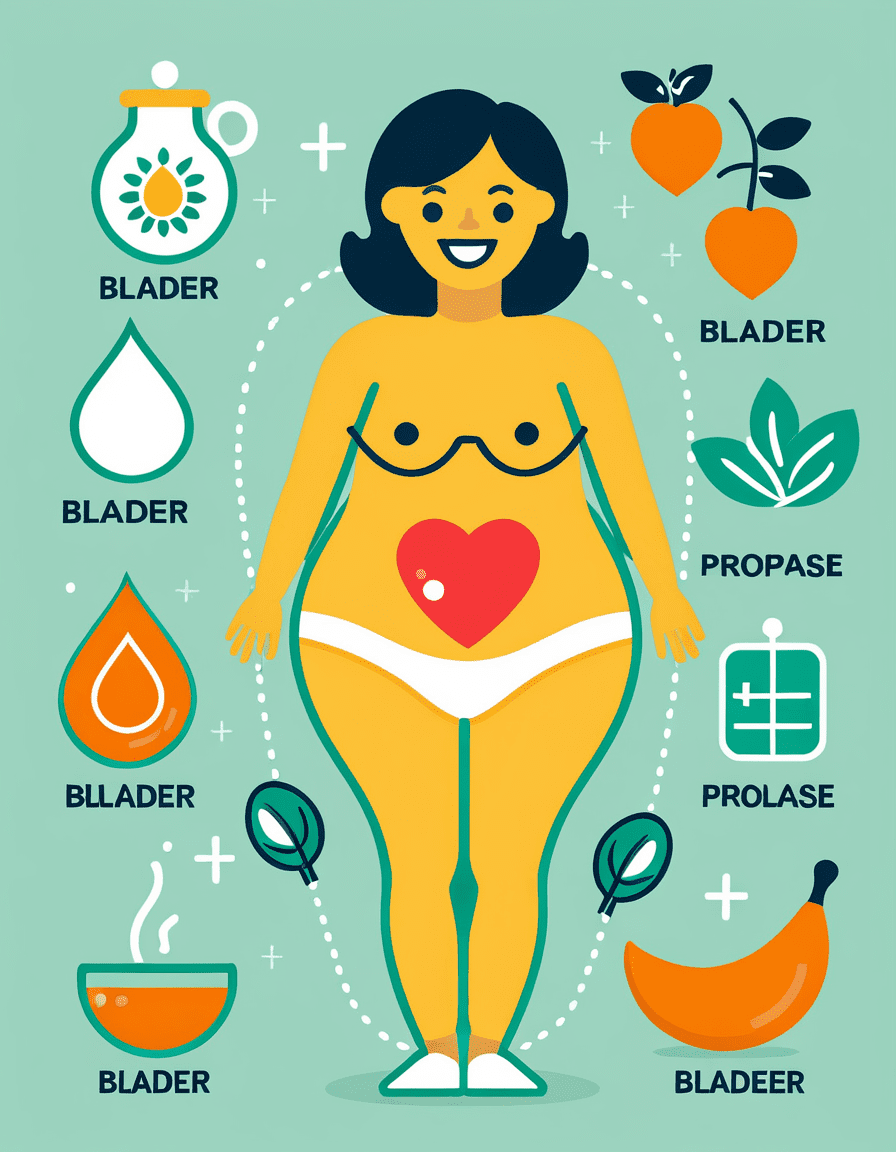
Bladder prolapse, or cystocele, is a condition many might not talk about, but it’s more common than you think. It happens when the bladder drops from its usual spot in the pelvis due to weakened pelvic floor muscles and tissues. This issue can hit hard, especially among women who’ve experienced childbirth, menopause, or various pelvic surgeries. With millions of people affected, it’s time to get the facts straight. Let’s dig deep into the causes of bladder prolapse and how they can impact your life.
What is Bladder Prolapse and Its Common Causes?
So, what exactly causes bladder prolapse? Various factors contribute to this condition, and understanding those reasons can lead to early intervention and effective management strategies. Here are the most prevalent causes:
Recognizing these causes is the first step toward effective management. The more you learn about bladder prolapse, the better you can take control of your health.

Top 5 Related Conditions Impacting Bladder Prolapse
Bladder prolapse often doesn’t come alone. There are several related conditions that can complicate matters, either co-occurring with it or sharing similar risk factors. Let’s break them down:
These non-cancerous growths develop on the cervix and can cause abnormal bleeding and discomfort. Women dealing with bladder prolapse often find themselves facing similar cervical issues, complicating their overall health picture.
Also happening alongside bladder prolapse, a prolapsed rectum can worsen urinary symptoms and lead to chronic pain. Just like bladder prolapse, rectoceles result from similar stress factors affecting pelvic positioning.
Commonly known as a benign tumor in the colon, tubular adenomas can trigger gastrointestinal symptoms. If you’re already grappling with bladder prolapse, these additional discomforts can feel overwhelming.
This infection leads to a painful collection of pus near the anus, causing further complications for those dealing with pelvic support issues. The discomfort may hinder everyday activities—a real challenge for anyone managing health concerns.
These seemingly unrelated cysts can create chronic oral pain and discomfort. Much like the persistent pain from bladder prolapse, oral mucoceles showcase how chronic issues throughout the body can enhance overall distress.
Knowing about these related conditions can sharpen your awareness and prepare you for discussions with your healthcare provider.
Managing Bladder Prolapse: Treatment Options and Lifestyle Changes
Addressing bladder prolapse isn’t just about tackling medical concerns head-on; it’s about integrating lifestyle changes that can make a major difference. Here’s a solid game plan:
1. Pelvic Floor Exercises (Kegel Exercises)
Strengthen those pelvic muscles! Regularly practicing Kegel exercises provides direct support for your bladder, potentially alleviating discomfort and improving your quality of life.
2. Physical Therapy
Consider specialized pelvic floor therapy. Professionals trained in this area can provide focused strategies to manage symptoms and help you regain pelvic support.
3. Pessary Devices
For non-invasive support, pessary devices offer effective solutions. These come in various shapes and sizes, designed to provide the bladder with extra support while you go about your day.
4. Surgical Intervention
When lifestyle adjustments and conservative methods aren’t enough, surgical options like anterior colporrhaphy come into play. This procedure repairs the vaginal wall that’s affected by prolapse.
5. Weight Management and Dietary Adjustments
Keep a healthy weight and eat a fiber-rich diet. These changes can help reduce strain during bowel movements and ease stress on your pelvic floor—creating a solid foundation for overall well-being.
Managing bladder prolapse is all about taking control and making informed choices that yield results.

The Emotional and Social Impact of Bladder Prolapse
It’s crucial to recognize that living with bladder prolapse goes beyond physical symptoms—there’s a mental and social component too. Many people report feeling embarrassed or reluctant to engage in social activities, and that can lead to isolation.
Support groups, like those offered by the National Women’s Health Network, create safe spaces for individuals to share experiences. They empower folks to discuss challenges and victories, fostering connection in a world that sometimes feels isolating.

Moving Forward: Reclaiming Quality of Life
Awareness surrounding bladder prolapse is expanding, and that’s fantastic news! With education comes empowerment. You’ve got the tools to live effectively with bladder prolapse, moving forward with confidence and strength.
Knowledge is your ally. The more you learn about managing bladder prolapse, the better equipped you become to navigate health challenges. Emphasizing a proactive approach with physical, emotional, and social health strategies can lead to a more vibrant quality of life for those affected.
As you gain insights about bladder prolapse, remember that you’re not alone. There’s a vast community out there ready to offer support and resources. With determination and the right knowledge, you can reclaim an active and fulfilling life—because that’s what it’s all about!
For further insights on health and wellness, check out related articles on genital Warts treatment, the latest on the Alabama Ivf ruling, or get updates like the latest Kate Middleton update. On your journey, you may even want to explore the spearmint tea Benefits for overall wellness.
Your health is your wealth—let’s keep building it!
Bladder Prolapse: Fun Trivia and Interesting Facts
Understanding Bladder Prolapse
Bladder prolapse, often dismissed as just another women’s health issue, packs more punch than most folks realize. Did you know that it can affect a staggering 50% of women who’ve given birth? And while childbirth is a common cause, aging and menopause can contribute significantly, too. For a broader perspective on how shared experiences shape health narratives, Anna Beth goodmans journey sheds light on personal stories linked to pelvic health challenges, resonating with many who face similar struggles.
Who’s at Risk?
It might surprise you to learn that factors like obesity and heavy lifting can increase the risk of bladder prolapse. Interestingly, many women might not even be aware they’re at risk until symptoms become evident. Now, combining everyday life with underlying health issues can sometimes feel overwhelming—something Chantal Andere knows all too well. Her unique take on health awareness showcases how having informed conversations can lead to better outcomes and greater community support.
The Connection to Daily Life
Living with bladder prolapse isn’t just about physical discomfort; it can really change how someone engages with the world. From social gatherings to trying out new activities, it can stifle spontaneity. This reminds us of the importance of light-hearted distractions, like scrolling through TikTok or keeping track of events on an April 2024 calendar for all those fun plans on the horizon! Despite the hurdles, it’s vital to remember that support networks and coping strategies can make a world of difference when navigating everyday challenges.
In sum, understanding bladder prolapse’s impact goes beyond just medical facts; it’s about acknowledging the multi-faceted experiences of those affected and knowing that help—and great stories—are always within reach.